Hormonal imbalances can cause disruptive symptoms such as hot flashes, night sweats, mood changes, and fatigue, leading many women to consider hormone replacement therapy. Yet, the difference between bio-identical hormones and the types commonly prescribed in conventional medicine often causes confusion, amplified by mixed research results and differing medical perspectives.
What Are Bio-Identical Hormones and How Do They Differ from Conventional Hormone Replacement?
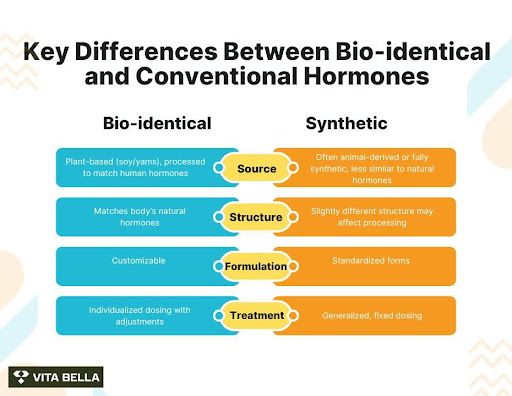
Bioidentical hormones are hormones that are recognized by the human body as the naturally produced hormones. They are used as treatment for people whose hormones are low or unbalanced. These hormones are typically derived from plant sources, such as soy or yams, and are developed in laboratories to match human hormones like estrogen, progesterone, and testosterone.
Difference between Bio-identical and Synthetic Hormones
Bio-identical hormones are chemically identical to the hormones naturally produced by the body, often derived from natural origin (plant-based). Synthetic hormones, used in traditional HRT, are either laboratory-made or animal-derived, such as Premarin, which is obtained from the urine of pregnant mares.
How Can Patients Navigate the Confusion Between Conventional and Bio-Identical Hormone Therapy?
Understanding the differences between conventional and bio-identical hormone therapy can be challenging. Misinformation, mixed research results, and conflicting medical opinions often leave patients uncertain. Conventional hormone therapy (CHT) uses FDA-approved, standardized products, but these often contain synthetic or animal-derived hormones that may not match the body’s natural hormones exactly.
In contrast, bioidentical hormone replacement therapy (BHRT) is custom-made to closely replicate each individual’s natural hormone profile, often using plant-derived ingredients. Supporters highlight that BHRT allows for personalized dosing and formulations tailored to specific needs, which some patients find more effective and better tolerated than standard HRT.
Questions to ask your doctor
Importance of individualized therapy
How to find reputable guidance and testing
By asking the right questions, focusing on your specific needs, and working with trusted professionals, you can cut through the confusion and choose a therapy that aligns with your health goals, comfort level, and long-term wellness priorities.
Why Was Hormone Replacement Therapy Demonized After the Women’s Health Initiative Study?
The Women’s Health Initiative (WHI) study, published in 2002, dramatically changed the way hormone therapy was perceived. The trial evaluated synthetic conjugated equine estrogens (Premarin) and synthetic progestins, not bio-identical hormones. Findings linked these synthetic formulations to increased risks of heart disease, stroke, blood clots, and breast cancer, which led to the study being stopped early and widely publicized in alarming headlines.
A critical issue was how the results were reported. The media emphasized relative risk percentages rather than absolute numbers, creating a perception of far greater danger than actually existed. For example, a “30% increase in risk” translated into only a small number of additional cases per 10,000 women annually, but this nuance was lost in public reporting.
As a result, millions of women and their doctors abandoned hormone therapy, and the stigma around HRT has persisted for decades. However, it is essential to note that these risks were tied to synthetic equine estrogens and progestins, not to bio-identical estradiol or micronized progesterone.
In fact, newer studies such as the KEEPS and ELITE trials show that bio-identical hormones can deliver cardiovascular and metabolic benefits when started early in menopause, while the E3N cohort demonstrated that micronized progesterone is associated with a lower cancer risk than synthetic progestins. This growing evidence confirms that bio-identical hormones provide a safer and more natural approach that should not be judged by the shadow of the WHI trial.
What Are the Benefits and Risks of Bio-Identical Hormone Therapy?
Symptom Relief and Quality of Life Improvements
Bio-identical hormone therapy (BHRT) is primarily utilized to alleviate symptoms associated with hormonal imbalances, particularly during menopause. Patients often report significant relief from symptoms such as hot flashes, night sweats, mood swings, and vaginal dryness. Additionally, BHRT may contribute to improved sleep quality and enhanced overall wellness. These benefits are attributed to the therapy's ability to restore hormone levels to those that closely resemble the body's natural state.
While BHRT is considered by many to be a safer alternative to conventional hormone replacement therapies, it's essential to recognize that all hormone therapies carry potential risks.
Furthermore, long-term use of hormone therapy4, regardless of the type, has been associated with an elevated risk of certain cancers, such as breast and endometrial cancer. Therefore, it's crucial for patients to engage in thorough discussions with their healthcare providers to weigh the potential benefits and risks before commencing treatment.
Are Bio-Identical Hormones Safer Than Synthetic Hormones?
Bio-identical hormones have gained increasing recognition among healthcare professionals and patients for their ability to restore hormone balance in a way that closely mirrors the body’s natural chemistry. Unlike conventional synthetic or animal-derived hormones, bio-identical hormones are structurally identical to those the human body produces, allowing for optimal compatibility, better symptom relief, and potentially fewer side effects.
When started at the appropriate time relative to menopause and tailored to the individual, research shows that bio-identical therapies, particularly estradiol and micronized progesterone, can deliver important health benefits that go beyond symptom control.
Key studies highlight several advantages of bio-identical therapy:
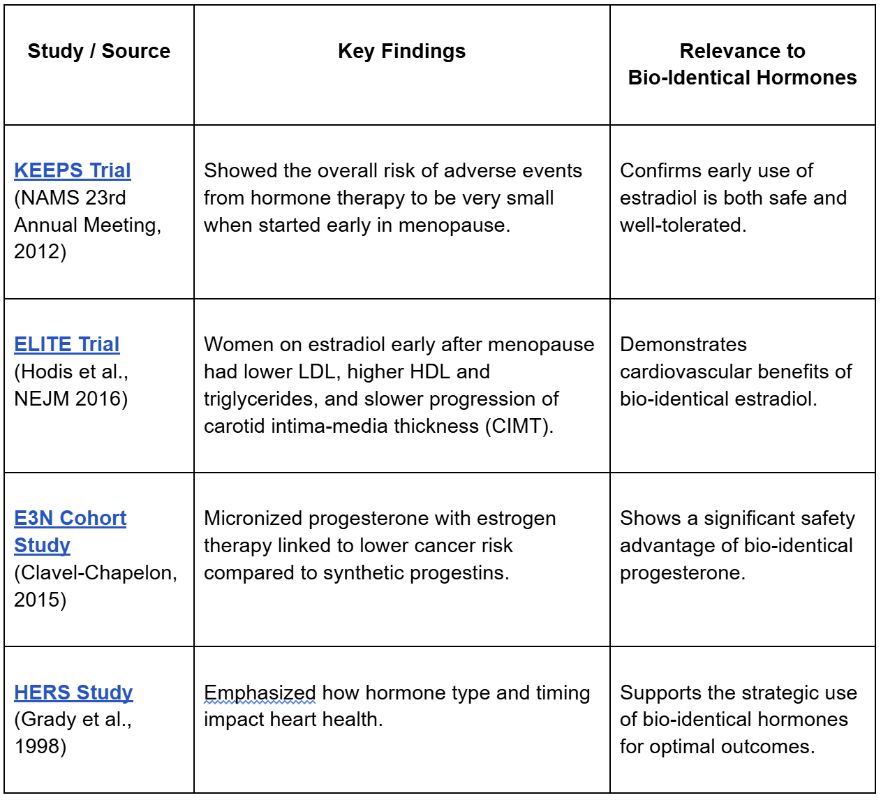
Taken together, these findings show that bio-identical hormones can deliver meaningful health benefits, improving cardiovascular markers, lowering certain cancer risks, and offering a safety profile that compares favorably to conventional synthetic options. For many women, bio-identical therapy offers a more natural, individualized, and well-tolerated approach to hormone balance.
Considering hormone therapy? Explore your options with Vita Bella and get a plan tailored to your needs
Many women face the discomfort of hormonal imbalance, hot flashes, night sweats, mood swings, fatigue, and weight changes, often unsure which therapy is safe and effective. At Vita Bella, we offer clarity and results with personalized bio-identical hormone therapy, supported by our range of premium wellness products designed to restore balance, relieve symptoms, and help you feel vibrant and confident again.
Frequently asked Questions
What are bio-identical hormones and how do they work?
Bio-identical hormones are hormones that have the exact chemical structure as those naturally produced in the human body. They are often used in hormone replacement therapy to balance hormone levels and reduce symptoms of menopause, PMS, or hormonal imbalances.
What are the benefits of bio-identical hormone therapy?
BHRT can help relieve menopausal symptoms such as hot flashes, night sweats, mood swings, and vaginal dryness. Many patients also report better sleep, increased energy, and improved quality of life when hormone levels are optimized.
How can I decide between bio-identical and conventional hormone therapy?
Consult a qualified healthcare provider who can review your medical history, symptoms, and risk factors. Understanding the differences can help empower you to make the best informed decision.
Do bio-identical hormones work better for symptom relief?
Many patients report that bio-identical hormones provide more consistent relief from hot flashes, mood swings, fatigue, and sleep disturbances compared to synthetic options. Because they match the body’s own hormones, they interact more smoothly with hormone receptors, often resulting in improved balance and fewer side effects.
References:
1- American College of Obstetricians and Gynecologists, Committee on Clinical Consensus–Gynecology. Compounded bioidentical menopausal hormone therapy. Obstet Gynecol. 2023 Nov;142(5):1266–73. doi: 10.1097/AOG.0000000000005395.
2- Cagnacci A, Venier M. The controversial history of hormone replacement therapy. Medicina (Kaunas). 2019 Sep 18;55(9):602. doi: 10.3390/medicina55090602.
3- Sibbald B. US estrogen plus progestin HRT trial stopped due to increased risk of breast cancer, stroke, and heart attack. CMAJ. 2002 Aug 6;167(3):294.
4- Stuenkel CA, et al. Compounded bioidentical hormone therapy: new recommendations from the 2020 National Academies of Sciences, Engineering, and Medicine. Menopause. 2021 Mar;28(5):576–578. doi: 10.1097/GME.0000000000001735.
5- Holtorf K. The bioidentical hormone debate: are bioidentical hormones (estradiol, estriol, and progesterone) safer or more efficacious than commonly used synthetic versions in hormone replacement therapy? Postgrad Med. 2009 Jan;121(1):73–85. doi: 10.3810/pgm.2009.01.1949.
6- Fournier A, Berrino F, Riboli E, Avenel V, Clavel-Chapelon F. Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort. International Journal of Cancer. 2005