What if healing after surgery didn’t have to take months? Pentadeca Arginate (PDA) could make that vision a reality. Pentadeca Arginate (PDA) is marketed as an arginate-salt form of the well-known pentadecapeptide BPC-157, retaining the same 15-amino-acid sequence. It has been used to aid in the healing of joint problems and partial tears of muscles or tendons.
Preparing for or recovering from surgery can feel overwhelming, but what if you could support your body’s natural healing from the inside out? At Vita Bella, we believe in merging science with wellness, and Pentadeca Arginate (PDA) represents that harmony perfectly. This clinically backed peptide is showing remarkable results in promoting faster healing, reducing inflammation, and enhancing tissue recovery both before and after surgery.
Why does PDA matter for surgery?
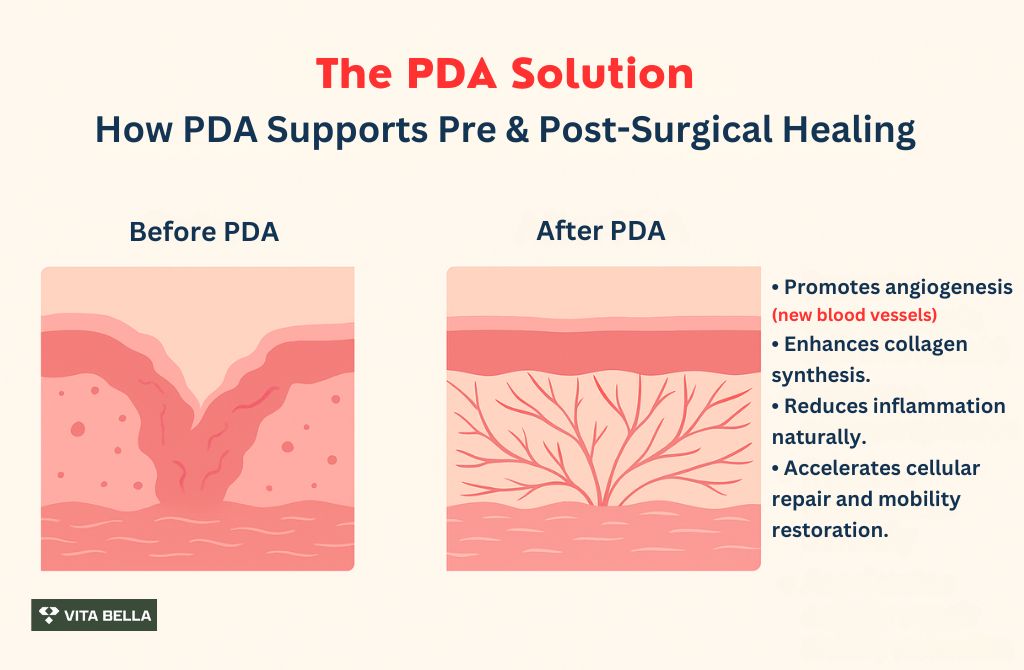
Pentadeca Arginate (PDA) supports one of the most critical aspects of surgical recovery: tissue regeneration and inflammation control. By promoting cellular repair and improving microcirculation, PDA may help reduce postoperative pain, speed healing, and enhance overall recovery outcomes without interfering with standard surgical protocols.
1- Clinically meaningful pain relief and functional improvement after a single injection
In a peer-reviewed retrospective human study 1 (n=16) of intra-articular BPC-157 for knee pain, 11/12 patients (91.6%) receiving BPC-157 alone reported significant pain improvement; overall, 14/16 (87.5%) improved, with benefits persisting beyond 3–6 months in most responders, findings that point to durable symptom relief relevant to post-operative rehabilitation timelines.
2- Rapid symptom resolution in a urologic pain condition (signal for mucosal healing).
According to study 5, during a single operation, the ladies had a cystoscopy and received injections of the peptide BPC-157 (10 mg total) in the bladder's inflammatory region. Intravesical BPC-157 (10 mg) injection for individuals with moderate to severe interstitial cystitis is being reported for the first time.
3- Tissue repair and angiogenesis pattern:
A 2021 review 2 highlighted BPC-157’s ability to accelerate wound healing and support incisional/excisional wounds, deep burns, and diabetic ulcers, noting its stability in human gastric juice and broader tissue-repair properties. Translating that to the surgical context means PDA may support earlier and more robust tissue repair, fewer scar‐tissue complications, and enhanced vascular support to healing beds.
4- Safety/tolerability in humans:
While high-quality human RCTs are lacking, existing evidence suggests favourable tolerability. For example, a narrative review 3 acknowledged the peptide’s high safety profile: “LD1 not achieved” in human‐translatable data and no serious adverse effects reported in the available human usage context. For perioperative use, this safety profile is a vital consideration.
How to Use PDA in the Pre- and Post-Surgical Pathway?
While formal guidelines do not yet exist for PDA, the human-data signals allow us to construct practical, hypothesis-driven frameworks for peri-operative use. Importantly, these should always be adjunctive to standard surgical care (analgesia, infection prophylaxis, and mobility protocols).
Pre-surgical (pre-habilitation) phase:
For patients with existing soft tissue or joint pain (e.g., knee, shoulder) entering surgery, PDA may help reduce baseline pain and improve tissue condition, which in turn could help improve pre-operative mobility and strength.
Because the knee-pain retrospective study 4 achieved 91.6% improvement in the BPC-157-only group, initiating PDA a few weeks pre-op could enhance baseline status.
Ensure coordination with the surgeon and anesthesiologist to confirm that peptide use does not conflict with perioperative anticoagulation or infection-risk monitoring.
Post-surgical (rehabilitation) phase:
After surgery, PDA may help reduce pain sensations, accelerate tissue repair, and support earlier functional milestones (e.g., earlier weight-bearing and range-of-motion goals).
Use in conjunction with physical therapy, analgesic tapering protocols, and wound-care monitoring.
Given the mucosal and wound-healing evidence 3 PDA could be particularly beneficial in surgeries where mucosal, vascular, or tendon healing is critical (e.g., bowel resections, ligament repairs).
Monitor outcomes such as pain scores, analgesic consumption, time to functional milestones, wound/repair integrity, and incidence of complications (e.g., delayed wound healing, infection).
How to frame PDA use around surgery?
With surgeon approval, PDA-class peptides could be positioned as an adjunct to ERAS-style pathways, not a replacement for evidence-based analgesia, infection prevention, or VTE prophylaxis, and discussed with attention to dosing, timing, and route. This approach ensures a comprehensive recovery plan that maximizes healing while maintaining standard care protocols.
Route matters: Intra-articular administration is aligned with joint-focused outcomes; intravesical dosing is aligned with bladder symptoms; IV data support feasibility when systemic delivery is preferred.
Duration matters: Single-dose effects lasting months suggest that evaluating PDA-class peptides during critical rehab windows to enhance participation and functional milestones potentially.
Accelerate Your Recovery: Discover Vita Bella's Surgical Benefits Today
Surgery can leave your body feeling drained, sore, and slow to heal. Prolonged recovery is often caused by inflammation, tissue damage, and compromised circulation, all of which hinder the body’s natural healing process. These issues can make even the simplest recovery feel like a significant obstacle.
At Vita Bella, we offer Pentadeca Arginate (PDA), a breakthrough peptide designed to accelerate recovery. PDA reduces inflammation, promotes tissue repair, and enhances circulation, helping your body heal faster and more efficiently. Start your recovery with Vita Bella and transform your healing journey into a faster, smoother process.
FAQs
Is Pentadeca Arginate (PDA) safe to use before and after surgery?
Yes, clinical studies on its core peptide sequence (BPC-157) show a strong safety profile in human trials, with no significant adverse effects reported. When used responsibly and under professional guidance, PDA supports healing and tissue regeneration without interfering with anesthesia, medications, or surgical outcomes.
Can PDA really speed up post-surgical healing?
Yes, research suggests that PDA promotes angiogenesis, collagen synthesis, and cellular repair, key factors in faster recovery. Patients in human studies reported reduced pain, improved mobility, and better tissue integrity, indicating PDA’s potential to shorten downtime and enhance the quality of post-operative healing.
Should PDA replace my prescribed post-surgery medication?
No, PDA is not a substitute for medically prescribed treatments or pain management protocols. Instead, it functions as a complementary supplement that supports the body’s natural repair mechanisms. Always consult your surgeon or physician before adding PDA to your recovery plan for optimal safety.
Is there clinical evidence supporting PDA’s effectiveness in humans?
Yes, multiple peer-reviewed human studies highlight positive results with peptides sharing PDA’s molecular structure, including improved pain scores, mucosal healing, and enhanced tissue recovery. These outcomes suggest PDA’s potential role as a powerful adjunctive option in both pre- and post-surgical care strategies.
References:
Seiwerth, S., Milavić, M., Vukojević, J., Gojković, S., Krezic, I., Batelja Vuletić, L., Horvat Pavlov, K., Petrovic, A., Sikiric, S., Vranes, H., Prtoric, A., Zizek, H., Durasin, T., Dobric, I., Knezevic, M., Sola, M., Kokot, A., Sever, M., Lovric, E., Skrtic, A., Boban Blagaic, A., & Sikiric, P. (2021). Stable gastric pentadecapeptide BPC 157 and wound healing. Frontiers in Pharmacology, 12, 627533. https://doi.org/10.3389/fphar.2021.627533
Sikiric, P., Seiwerth, S., Skrtic, A., Staresinic, M., Strbe, S., Vuksic, A., Sikiric, S., Bekic, D., Soldo, D., Grizelj, B., Novosel, L., Beketic Oreskovic, L., Oreskovic, I., Stupnisek, M., Boban Blagaic, A., & Dobric, I. (2025). Stable gastric pentadecapeptide BPC 157 as a therapy and safety key: A special beneficial pleiotropic effect controlling and modulating angiogenesis and the NO-system. Pharmaceuticals, 18(6), 928. https://doi.org/10.3390/ph18060928
Lee, E., Walker, C., & Ayadi, B. (2024). Effect of BPC-157 on symptoms in patients with interstitial cystitis: A pilot study. Alternative Therapies in Health and Medicine, 30(10), 12–17. https://doi.org/10.1016/j.alth.2024.08.002
QUICK SUMMARY:
Here are the key takeaways from the document about Pentadeca Arginate (PDA) for surgery:
What is PDA? It's basically a salt-form of the well-known peptide BPC-157. It has the same 15-amino-acid structure and is marketed to help with things like joint issues and partially torn muscles or tendons.
The Big Idea: Imagine healing way faster after surgery—not months, but quicker. PDA aims to help your body's natural healing process by boosting tissue regeneration and calming down inflammation both before and after you go under the knife.
Why it's a Big Deal for Surgery:
Pain Relief & Better Function: A study on knee pain showed that most patients (over 87%) who got BPC-157 had serious pain improvement and better function that lasted months. Starting PDA before surgery might even improve your baseline condition.
Supercharge Tissue Repair: It’s known to speed up wound healing (like cuts, burns, and ulcers). For surgery, this means potentially stronger repairs, less scarring, and better blood flow to the healing area.
Good Safety Vibe: Current human evidence suggests it has a good safety profile with no serious side effects reported. That’s a huge plus when you're dealing with surgery.
How to Use It (Think of it as a teammate, not a replacement):
Before Surgery (Pre-hab): If you already have joint or soft tissue pain, starting PDA a few weeks beforehand might reduce pain and make your tissue healthier, potentially leading to better mobility and strength before the operation. Crucial: Always get the green light from your surgeon and anesthesiologist first!
After Surgery (Rehab): It can help reduce pain, speed up tissue repair, and help you hit those rehab goals (like walking sooner or getting back your range of motion). It’s especially helpful for surgeries involving mucosal, vascular, or tendon healing (think bowel or ligament repairs).
Remember This:
It's an Adjunct: PDA is there to support your recovery plan (like physical therapy and pain management), not replace your prescribed medications, infection prevention, or blood clot protocols. Don't ditch your meds for PDA!
Consult Your Pro: Always talk to your surgeon or doctor before adding PDA to your plan to make sure it's safe and right for you.





















