There are many cases reported each year related to patient safety associated with sterile drug manufacturing, compounding, and administration. However, sterility assurance was the main goal of past regulations. But many compounding errors compromise the sterility of medicine 1. To determine and lower the likelihood of such errors and the factors that contribute to them, further initiatives are needed.
Your health deserves uncompromised safety. At Vita Bella, we make sure every medication is prepared, stored, and delivered under the strictest sterile standards. Trust us to protect what matters most, your well-being. Choose Vita Bella for sterility you can count on.
Why Sterility Matters in Every Route of Drug Delivery.
In view of the sterility situation, the Institute for Safe Medication Practices (ISMP)2 organized a meeting of 60 experts in the field in October 2011 to develop consensus directions, safe practices, and standard operating procedures for the safe preparation and compounding of sterile preparations, particularly intravenous admixtures.
Administering medicines to a patient in a sterile manner involves prevention of microbial contamination. There are different routes through which a medicine can be administered to the body.
Routes of administration include oral, intravenous subcutaneous, intramuscular, and topical. In addition to convenience, the drug's characteristics and pharmacokinetics influence the methods that are used to administer the drug. Considering the distinctive qualities of the different routes and different strategies are required to maintain sterility and avoid contamination of medication.
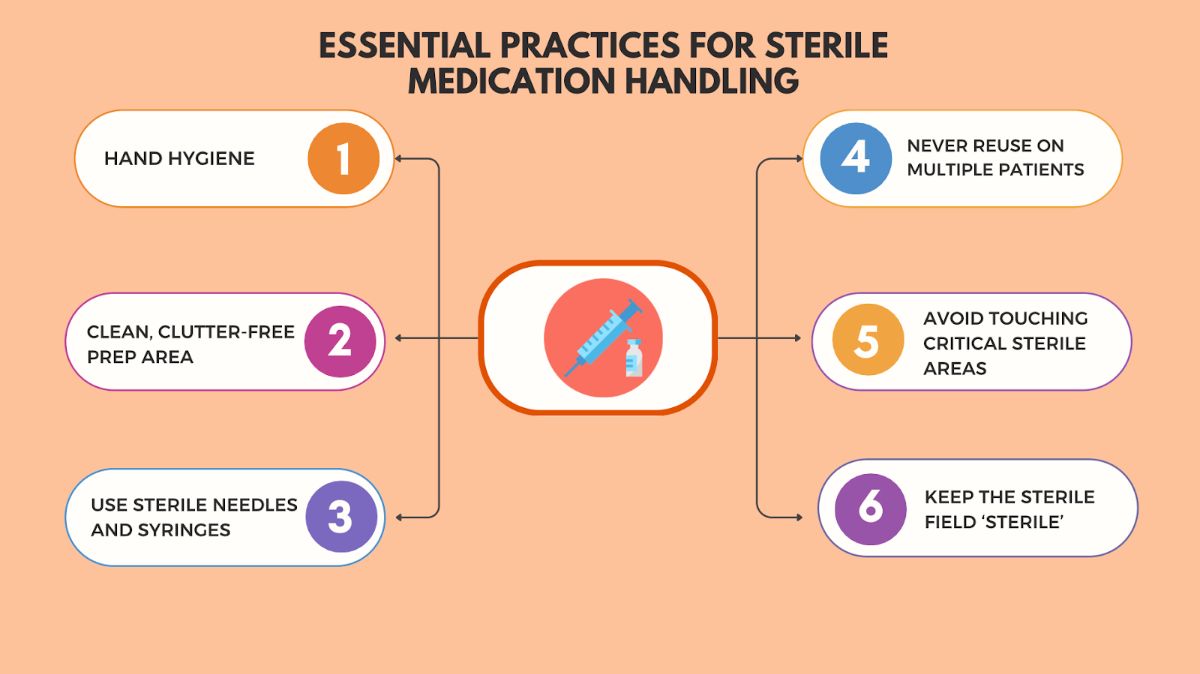
Essential Practices for Sterile Medication Handling
The majority of medicines we use are sterile mixtures. ISMP has discovered a number of additional concerns for sterile and compounded medications through the investigation of related complaints it receives from various hospitals. Multiple steps must be taken to ensure that medicines are safe to use, including strict hand hygiene, handling of devices, strictly following practices to avoid contamination, and most importantly, strict sterility rules. Lets dive in deeper.
1. Hand Hygiene
Healthcare professionals strictly follow hand cleanliness as it is said to be the best possible method of limiting the transmission of microbes. It includes hand sanitizers, antiseptic hand rubs (alcohol-based foams or gels), and hand washing with soap and water. The "Five Moments for Hand Hygiene"4 are a set of standards established by the World Health Organization (WHO) that specify when hand hygiene is required.
It is necessary to clean hands before and after preparing, administering, and injecting parenteral with any of the approved hand hygiene methods.
2. Clean, Clutter-Free Prep Area
Medicines for injection 5 should be prepared in a clean and designated sterile area. Before and after usage, wipe surfaces with 70% isopropyl alcohol, then allow them to dry. Ensure the sterility of the syringe and parts of the needle. The items shouldn’t be removed from packaging just before their use and they should never be reused. Maintain the sterility of the tip of the syringe and cover it with a needle or cap. Keep the needle away from non-sterile surfaces like the counter, the needle cap's surface, and the outside edges of the vial or ampule. Always keep the needle covered with a cap unitl use and keep your hands away from the plunger's length when not in use.
3. Use Sterile Needles and Syringes Every Time
It is prohibited to use one loaded syringe to give medicine to several patients (i.e., make sure you have one needle, one syringe, and one patient). Fill the drug from the ampoule or vial using a sterile syringe and needle. That's why, before administering and reconstituting a medicination open a new sterile syringe 6.
4. Never Reuse on Multiple Patients
When using multiple doses of a medication the medication should never be shared with another patient even if you are on taking same medication and does as this increase risk of contamination and transmission of communicable diseases.
5. Avoid Touching Critical Sterile Areas
Needles, catheters, and syringe tips are critical locations for materials having a sterile surface. They must always be maintained sterilely 8. It is possible to improve non-touch operation to avoid crucial areas coming into contact with non-sterile surfaces. The primary issues were considered to be inadequate ways of disinfecting non-sterile objects and the possibility of contacting sensitive areas. There was little chance of non-sterility through the aerial route.
6. Keep the Sterile Field ‘Sterile’
It is very important to maintain the integrity of the sterile field, no matter whether you're working on a tray or a countertop, by keeping it visible, over waist level, and away from non-sterile areas. A key aspect of medicine safety for parenteral products is its sterility. The FDA recommended Current Good Manufacturing Practice (CGMP) 9 rules to set minimum manufacturing standards and offer regulatory guidelines for the production of high-volume parenteral medicines.
FAQS
1. Why is hand hygiene so important before giving medications?
WHO and CDC both emphasize hand hygiene as the most useful infection prevention method in medical administration. Because hand hygiene kills viruses and bacteria, it leads to bloodstream infections when transmitted through IV lines and IV injections.
2. Can the same syringe be used for more than once if the needle is changed?
No. Using the same syringe over and over, or after changing the needle, increases the likelihood of contaminating the drug via. Every administration needs a new needle and syringe.
REFERENCES
3. Kim, J. and O. De Jesus, Medication routes of administration. 2021.





















