Thinking of starting TRT or peptide therapy? Imagine adjusting your dose blindfolded with no lab tests; that’s what many do. Lab tests are essential because they establish a clear picture of endogenous hormone levels, metabolic health, inflammation, and organ function key data that guide safe, personalized therapy1.
Metabolic panels (glucose, liver/kidney function) detect underlying conditions that could amplify side-effects2. Low testosterone 3 and inflammation are both associated with chronic illnesses like cardiovascular disease, men may be evaluated for C-reactive protein (CRP) and inflammatory cytokines like IL-6 prior to beginning TRT. All three adiposity metrics (waist circumference, body fat percentage, and BMI) showed a favorable correlation with serum IL-6 in terms of inflammatory status. Contraindications (e.g., existing cardiovascular disease, prostate issues) may be missed, increasing the chance of harm4. Baseline labs promote efficacy5 , safety, and personalization.
Your health isn’t one-size-fits-all, why should your treatment be? At Vita Bella, we utilize in-depth lab testing to create personalized TRT and peptide protocols tailored to your needs. Take the first step toward balanced hormones, better energy, and long-term benefits.
Why Baseline Labs Matter Before Starting TRT Therapy
According to the Endocrine Society Clinical Practice Guidelines 6, it was suggested that using precise assays and measuring associated hormones, such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), and morning total testosterone levels, can be done to confirm low testosterone.
Labs also reveal metabolic health7 status: studies link low baseline testosterone to higher risk of metabolic syndrome and type 2 diabetes. In a cross-sectional/longitudinal study, men with lower serum T had significantly higher odds of being diabetic or having metabolic syndrome.
Checking baseline labs for organ function and safety7 (CBC, liver, kidney, PSA, etc.) helps identify contraindications or issues like anemia, prostate disease, or kidney impairment. Guidelines (e.g., Endocrine societies) emphasize that many men begin TRT without even confirming low testosterone in lab tests first. Up to 25% of men who receive TRT may not have had their T levels tested before initiation.
Without labs: risk of overtreatment (leading to polycythemia / high hematocrit), worsening insulin resistance, liver strain, or missing underlying disease that could be dangerous under hormone therapy. Baseline lab values allow dose personalization, monitoring, and minimizing side effects.
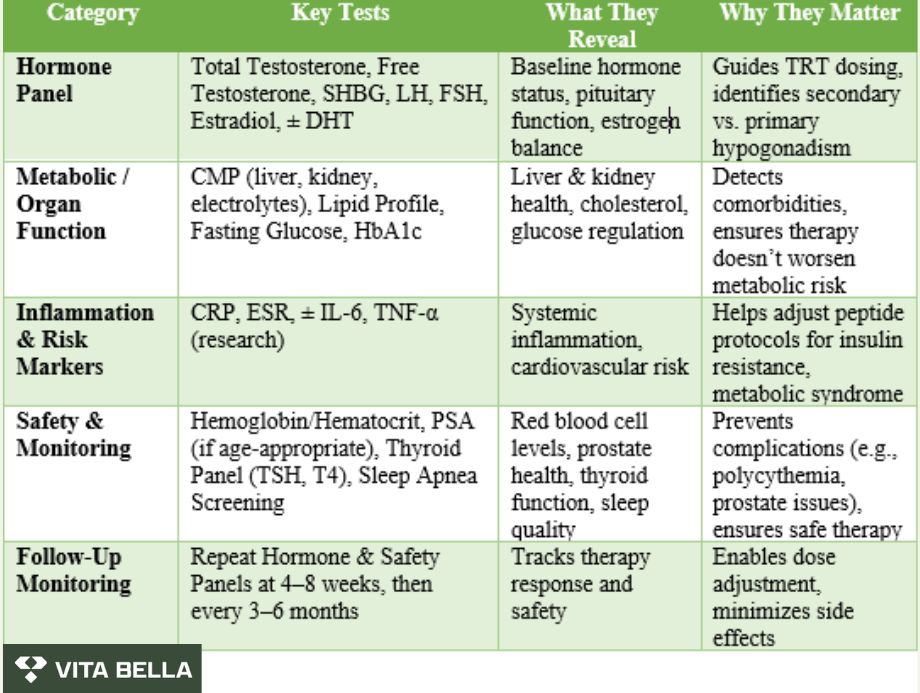
Key Lab Panels You Need for TRT and Peptides
The following are the key lab panels you need before starting TRT therapy, including hormone, metabolic, inflammation, and safety labs. Key lab panels are essential for personalizing TRT, balancing risk, and maximizing benefit. According to the AUA Testosterone Deficiency Guideline, the hormone panel should include total testosterone (measured in the morning, twice), free testosterone, SHBG, LH, FSH, and estradiol to confirm deficiency and understand pituitary vs testicular contributions.
Metabolic panels, like a comprehensive metabolic panel (CMP)8, fasting glucose or HbA1c, and lipid profile, help assess baseline metabolic health. These detect potential insulin resistance or liver/kidney impairments that could affect dosing and safety.
Critical Labs to check for safety: hemoglobin and hematocrit to watch for erythrocytosis (e.g. one study found 57% of patients on TRT reached hematocrit > 0.46 after therapy). Prostate Specific Antigen (PSA) and digital rectal exam if age-appropriate; and thyroid labs (TSH, T4) to rule out other endocrine contributors8.
How Labs Guide Personalized TRT & Peptide Protocols
1- Tailoring dose & form (injections, creams) based on hormone baseline:
Choice of formulation12 (creams and injections) depends on baseline testosterone levels and patient preference. Different forms have different pharmacokinetic profiles and different half lives; e.g. injectable testosterone cypionate vs propionate - knowing how a patient is metabolising these medications based on labs helps to dial in the therapy.
2- Adjusting peptide selection/dose based on metabolic health:
GLP-1 analogs help manage insulin release and enhance the body's glucose processing when treating metabolic disorders13. Since improper dosing in patients with renal dysfunction can result in toxicity or ineffective therapy, dose adjustments for peptide14 medications may be necessary for patients with renal impairment to prevent accumulation and increased drug exposure.
3- Monitoring frequency: when & what labs to repeat:
To achieve therapeutic levels between 450 and 600 ng/dL, the preparations based on the pharmacokinetic dosing principle of measuring steady state have varying times for monitoring testosterone levels 8. Patients who see a restoration in total testosterone levels but do not see a change in symptoms or signs 3–6 months after starting treatment should think about stopping TRT.
From Lab Results to Life Results with Vita Bella
Many men struggle with fatigue, weight gain, or low stamina, yet jump into TRT or peptide therapy without proper lab testing risking side effects, missed diagnoses, or ineffective treatment. At Vita Bella, we do things differently. We begin with comprehensive laboratory tests to assess your hormone levels, metabolic health, and inflammatory status.
This scientific foundation allows us to create, personalized TRT and peptide protocols that not only boost energy but also protect your long-term heart and metabolic health. With Vita Bella, you’re not guessing you’re transforming your health with precision and confidence.
FAQs
1: Why are baseline lab tests essential before starting TRT or peptide therapy?
Baseline labs confirm whether testosterone deficiency is real, rule out underlying conditions, and provide a safety benchmark. They measure hormone levels, metabolic health, and organ function, ensuring that therapy is personalized, effective, and safe.
2: Which lab tests are typically recommended before TRT or peptide protocols?
Doctors usually recommend morning total testosterone, free testosterone, SHBG, LH, FSH, estradiol, CBC, PSA, liver and kidney panels, glucose/HbA1c, and lipid profile. Inflammatory markers like CRP or IL-6 may also be checked to assess metabolic and cardiovascular risk.
3: How do lab results guide the personalization of TRT and peptide therapy?
Lab results determine whether TRT is needed, the safest starting dose, and the right form (injections, creams, etc.). For peptides, labs help identify metabolic issues, insulin resistance, or visceral fat levels, allowing adjustments in dosage and peptide choice. Follow-up labs, then track progress and fine-tune protocols.
References:
Bhasin, S., Brito, J. P., Cunningham, G. R., Hayes, F. J., Hodis, H. N., Matsumoto, A. M., Snyder, P. J., Swerdloff, R. S., Wu, F. C., & Yialamas, M. A. (2018, March 19). Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. Endocrine Society. Retrieved from https://www.endocrine.org/clinical-practice-guidelines/testosterone-therapy





















